Major depressive disorder patient recruitment for clinical trials
Need help accelerating your study?
Depression is estimated to affect 264 million people worldwide, yet trials still face problems with recruitment.
Depression is set to become the world’s largest health problem and primary cause of disability by 2030, surpassing cardiovascular disease, cancer, and diabetes. Despite affecting mainly young people online, it remains difficult to reach and enroll them in clinical trials, posing a challenge for organizers. Targeting the right audience is also crucial to reduce placebo response rates.
Having supported 10+ psychiatric studies (from Phase I-IV). With our multichannel digital marketing approach (that covers 40+ channels), patient insight expertise, depression community analysis and study protocol reviews, we can solve your patient recruitment challenges.
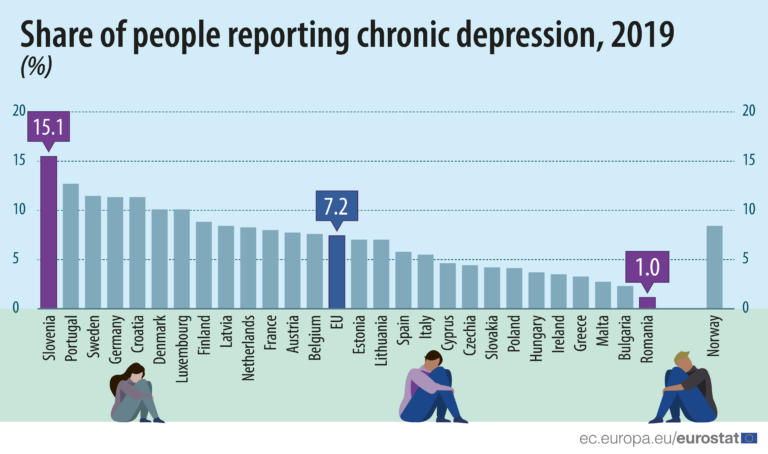
Prevalence of depression around the world
The prevalence varies widely across different nations and local communities, socioeconomic backgrounds, ethnic and racial backgrounds, age groups, as well as gender identities.
Even before the start of the pandemic, the chronic depression rates in the European Union were on the rise. In 2019, 7.2% of EU citizens reported having chronic depression. In the US, these rates are even higher.
Image source: European Commission, Eurostat
Reach people with depression who are more likely to qualify and less likely to drop-out
There is widespread reluctance to seek help for depression, with only a small majority (57%) seeking help from professionals. In addition, because physicians and psychologists may be unaware of ongoing clinical trials, or simply reluctant to refer patients to clinical trials, digital outreach is critical to reaching those with depression.
Patient-centric content that informs patients about the possibilities, as well as how much time and effort participating may take, helps increase participation rates.
Research has shown that the most common reason people with depression do not seek help or participate in trials is the perception that they have to deal with their own problems, along with the stigma of participating in clinical trials. By providing understandable explanations about clinical trials and the treatment of depression, and highlighting the fact that many people choose to participate in depression trials for a variety of reasons, we work to increase health literacy and build trust. This ultimately leads to higher participation and lower drop-out rates.
Dropout reduction: Clinical trials for the treatment of depression have among the highest drop-out rates of all clinical trials. For many participants, mood swings or a low mood in general, are reasons to cancel study appointments. By reminding patients in advance, we help them prepare for study visits. Information on the need for and benefits of clinical trials for individuals, medicine, and society also encourages continued participation.
Find patients aligned to your protocol
Depression is typically diagnosed according to the DSM-5 and, for clinical studies, using the Hamilton Depression Rating Scale (HAM-D). Depending on the severity of symptoms, depression is categorized as mild, moderate, or severe. For example, in many depression clinical trials targeting severe cases (or wanting to limit the placebo response rate), the inclusion criterion is a total HAM-D score of 18+ points.
Some forms of depression may also be more constant or chronic or may occur with or without manic episodes. These different categories, and the symptoms that define them, can be used as indicators to find patients who are both likely to qualify and less likely to fail. At the same time, researchers have pointed out that, similar to the diagnosis of heart failure, for example, there is no clear diagnostic method for depression. Moreover, in recent studies, researchers also found that patients with similar diagnoses of depression still have very large differences in response to treatments.
Our Chief Medical Officer reviews your protocol and aligns with our patient recruitment team’s objectives and tactics to ensure that patients referred to your research center fit the requirements of your study. We can suggest a set of inclusion and exclusion criteria for your depression study and then build our multichannel outreach campaign based on your criteria.

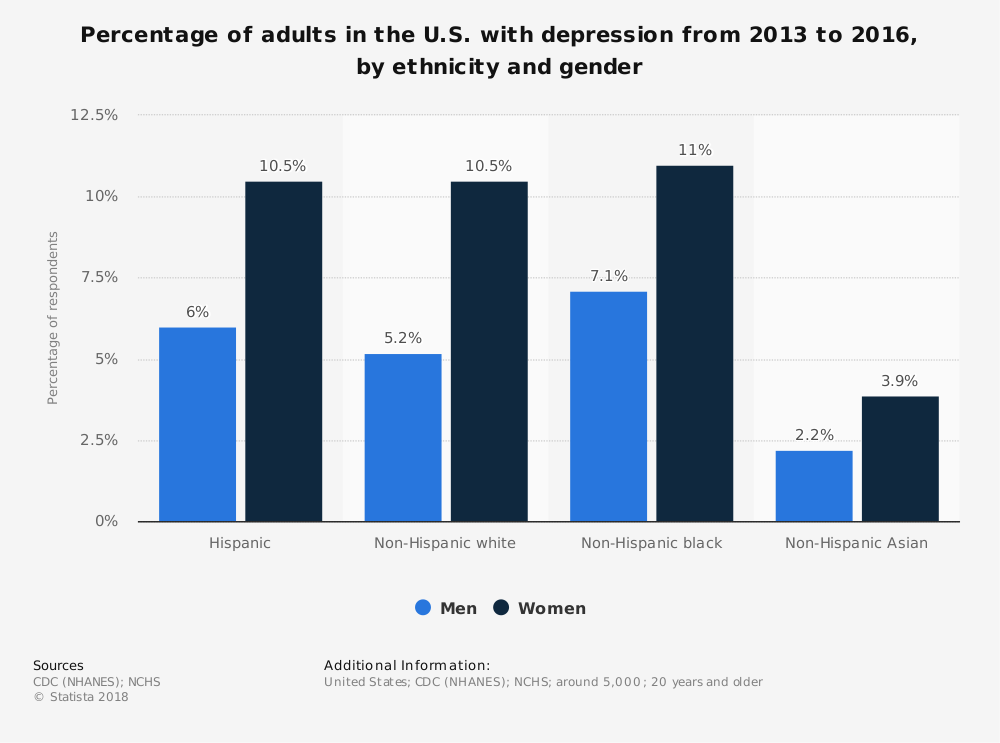
Addressing patient diversity
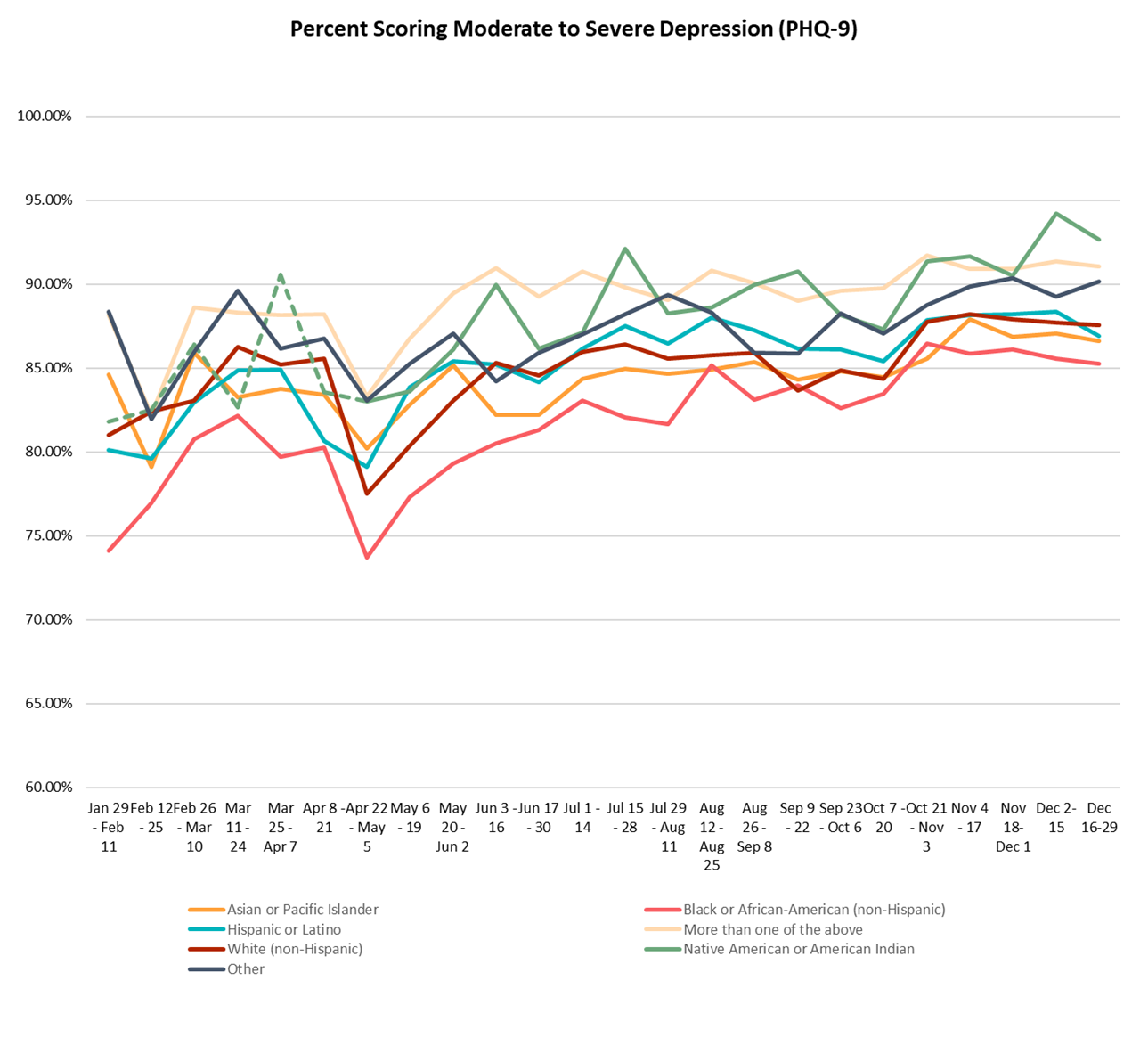
Minority groups are underrepresented in all clinical trials, including studies on depression. In recent years, research has increasingly focused on including ethnic minorities, people with different gender identities, and trauma survivors in clinical trials on mental illnesses, such as depression. To date, however, these efforts have not been overly successful – despite the fact that ethnic minorities are increasingly seeking professional help for their condition. For example, in the USA, there was a large increase in Asian and Pacific Islander (17% increase in the study population), as well as Native Americans (7.5% increase) and African Americans (6.89% increase) seeking help for their depression in 2020.
Sponsors of clinical trials in depression have increasingly sought to globalize their studies over the past decade. Including patients and physicians worldwide addresses patient diversity, increases patient recruitment in many developing countries, and allows for earlier access to new therapies and medications. Patients with depression in developing countries typically do not have adequate access to treatments and are less likely to have used existing antidepressants. This also means these patients may respond better to newly developed antidepressants as they are naive to current treatments.
We help identify and reach a diverse patient population with customized languages, study information, and study advertisements. In this way, we are able to recruit a representative population for your depression studies.
Based on patient insights, we can reach a more diverse patient population with our patient recruitment and retention services.. We use digital tools and multiple communication channels to reduce physical barriers to accessing the study site, create patient-friendly study materials to increase health literacy, and adapt our strategies to local communities and cultures.
By understanding patient needs, we can overcome the unique barriers these patients face when enrolling or participating in clinical trials.
Our digital targeting techniques
Demographic targeting
Age, social media behavior and profile, and other demographic indicators are used as filters to find people with depression (and their families) that are most likely to match your study.
Age, in particular, is an important factor. Where major depression affects more people between the ages of 45 and 65, severe depression is more likely to affect the very young and very old.
Low socioeconomic status has also been linked to a higher prevalence of depression (based on education, rather than income; Freeman, 2016).
Location & capacity targeting
We consider geographic variation in depression prevalence. Therefore, patients living within a predesignated radius around active sites are targeted with ads that are activated and deactivated based on site referral volume.
For example: In the USA, researchers conclude that there is no significant difference between the prevalence of depression in rural areas and cities. However, in Germany, rural areas with a low population density showed the highest prevalence (+34%), while big urban municipalities showed the lowest (+25%).
Interest-based targeting
Gender, ethnicity, socioeconomic People with depression are primarily young and active online. Through forums, social media groups, and events, we reach out and explain the processes and potential benefits of participating in clinical trials.
Database & Behavioral targeting
We send study notifications to our large database (>1.3 million registered ClinLife users worldwide) based on their location and indication details. By continuously analyzing the (anonymized) behavior of those who were successfully enrolled, we can understand and reach similar people.
Are you designing a depression study, or have one underway?
We can help you find the right patients, at the right time. To find out more about our depression patient recruitment, contact us.