Organizers of clinical trials for heart diseases for long have struggled finding and retaining the required number of patients to participate in their trials. Recently conducted meta-reviews suggest, that recruitment for heart trials is often more difficult then for other indications.
In our last blog we looked at how organizers of cardiovascular disease trials can overcome the 4 leading barriers to cardiovascular disease patient recruitment. In this blog we will compare traditional versus digital methods of patient recruitment for cardiovascular disease clinical trials.
Drawing on our more than 16 years of experience in which we supported over 70 cardiovascular disease clinical trials around the world, we demonstrate how data-driven digital patient recruitment can solve many of the recruitment issues that organizers of cardiovascular disease trials face. At the same time, we also briefly look at common mistakes with digital patient recruitment.
This blog will look at:
- Traditional methods of patient recruitment for cardiovascular disease
- Digital methods of patient recruitment for cardiovascular disease
- Common mistakes in digital patient recruitment
- Our approach to digital patient recruitment for cardiovascular disease studies
This blog is based on our recent whitepaper in which we reviewed the most recent literature on patient recruitment for different cardiovascular diseases. Download the free cardiovascular disease recruitment whitepaper here.
1. Traditional methods of patient recruitment for cardiovascular disease
Organizers of clinical trials have historically strongly relied on primary care practices, doctors and hospitals to get potential participants for their clinical trials. This has both advantages and disadvantages.
- Advantages: doctors know the diagnosis of patients, are in direct contact with them and have established a relationship of trust.
- Disadvantages: It depends entirely on doctors’ proactive measures and knowledge about clinical trials. If doctors are not aware of available trials or only take care of a limited group of patients, this does not contribute significantly to overall enrollment.
With increased attention to the importance of diversity and representation in clinical trials in recent years, it has become clear that physician practices are generally able to refer white and highly educated patients, but not underrepresented groups such as ethnic minorities. This is especially true in countries such as the United States, where minority populations often lack access to good health care providers.
Yet, as recent studies suggest, it might also simply be a misconception under organizers of clinical trials for cardiovascular disease is that traditional methods of recruitment give a higher quality of referrals”. Although the assumption that primary health care professionals know the patient better and therefore are more aware who they should and shouldn’t refer sounds logical, recent reviews by for example Mary McGrae McDermott et al (2016) show that this is not the case. As McDermott writes:
“Of the 372 patients with peripheral artery disease referred from primary care practices, only 23 (6%) were randomized, representing just 10% of the total number we needed for the trial”
– McDermott et al (2016).
As we highlight in our free academic white paper (14 pages) on patient recruitment in cardiovascular disease, reviews, e.g., by Harrison et al. (2018), show that even cardiac patients referred by physician practices often ultimately decide not to participate in clinical trials because they are not adequately informed.
The effectiveness of other forms of traditional patient recruitment such as offline marketing, such as advertisements in newspapers, public transport or street posters was already increasingly questioned before the pandemic, but has been clearly proven outdated since the big changes brought about by the COVID-19 Pandemic. However, an often overlooked problem with traditional patient recruitment is the complete inability to target patients who are likely to qualify and be randomized.
2. Digital Patient Recruitment for cardiovascular disease clinical trials
Digital patient recruitment is becoming an increasingly discussed topic in scientific journals and generally refers to one of two methods that are almost always used in isolation.
- Direct outreach: cardiovascular patients are pro-actively reached with for example display ads on social media platforms as Facebook, Instagram and TikTok or other digital platform.
- Indirect targeting: cardiovascular disease patients or their families and friends search online about their diagnosis, indication, treatment options, or the possibility of participating in clinical trials for heart disease and find our patient-centric ClinLife® platform themselves.
3. Common mistakes in digital patient recruitment for cardiovascular disease trials
While direct targeting sounds straightforward, in order for it to be cost-effective and help patients be not just referred but also randomized, a lot of experience and know-how is required. Otherwise, a recruitment campaign can quickly go astray, resulting in study site staff being overwhelmed with workload of screening referrals, budgeting issues for outreach efforts, few to no randomizations or a high number od dropouts and thereby delays to the study.
Without a good understanding of the patient population, an effective and patient-friendly pre-screener, and data-driven outreach methods, it is very likely that referrals will not be randomized due to increasingly strict exclusion criteria.
To summarize, digital patient recruitment without a strategy based on experience, understanding of the patient population and data-driven methods might lead to some referrals but also to:
- A unnecessary high cost for referrals
- High workload for the site staff
- Frustration and disappointment by patients for not being able to take part
As patient centricity becomes increasingly important in clinical research, it is critical to incorporate it into patient recruitment campaigns and reduce the likelihood that patients will be told at their initial screening visit that they cannot participate. Indeed, bad experiences in the enrollment phase may be a reason for patients not to want to or be able to participate in clinical research in the future.
4. Digital patient recruitment for cardiovascular done right: our experience
Based on our experience of 16+ years with digital patient recruitment including a variety of cardiovascular diseases, we know that digital patient recruitment can be more effective than traditional methods, enroll more patients under budget and most importantly, provide patients with a good experience with clinical research. This is not just important because these patients then feel part of scientific accomplishments, but also practically because they are more likely to join future stories or tell friends, family or other patients of their experiences.
What patients say:
“I usually never click on ads, but this ad about a clinical trial really appealed to me, so I applied right away. The research centre was only 2 km away, so the personal approach was optimal.”
– 2021 Patient’s Voice Participant
In the understanding graphics it becomes clear that a data-driven digital patient recruitment approach for Cardiovascular Diseases has to make use of a variety of different ads and platforms. For commercial sensitivity reasons we cannot specify the different Google ads and smaller channels, but depending on the campaign we use up to 40+ different digital channels.
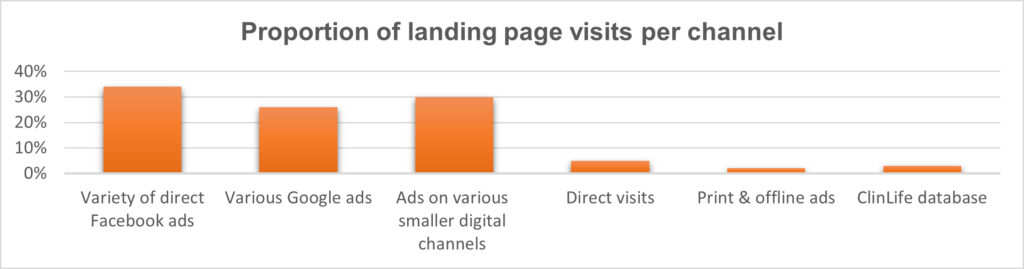
More so, while the ClinLife® database is only a small portion of the landing page visits, for cardiovascular disease campaigns it on average leads to 30% of the referrals we contribute.
Our approach to digital patient recruitment for Cardiovascular Disease trials
1. Customizing the patient profile based on study criteria: Depending on the type of cardiovascular disease and location of the site, we create a detailed patient profile based on the study protocol.
When necessary, we also define the need to reach potential caregivers and other family members or contacts. Through analysis of social media responses and questions, large-scale surveys and qualitative interviews, our Patient’s Insights Team can create an overview of the needs and wishes of the local patient group.
2. Individualized targeting: patients likely to qualify are shown advertisements depending on their proximity to the study center.
3. Behavioral targeting: data-driven algorithms identify people with similar online behavior to those who have already successfully registered for the study or people who visited the study site but did not register. This allows for the a targeted approach to people who are likely to pass the pre-screener.
4. Lay-friendly information, study material: one, if not the most important factor influencing peoples Willingness to Participate (WTP) in clinical trials is understanding and trust. For this reason our ClinLife® platform is designed in direct collaboration with patients for other patients. From the study or indication landing page with patient-friendly information about clinical trials and research into cardiovascular diseases and new medications, therapies and treatment options, to the explanation of the study procedure.
5. Study specific or indication specific pre-screener: depending on the type of recruitment campaign either a study specific or indication specific pre-screener with easily understandable questions that make sure only people likely to qualify are referred.
For more details on how these methods can be employed for cardiovascular diseases as stroke, heart failure and atrial fibrillation, download our free cardiovascular disease whitepaper here.